| |
Varicoceles |
|
|
The male reproductive tract is responsible for the production, maturation, and transport of sperm. This tract is a complex and highly integrated entity. Sperm produced in the testicles are transported through the genital duct system and deposited in the urethra during ejaculation followed by emission.
Abnormalities within the male reproductive tract may present as a scrotal masse. Masses may have little or no health significance or may represent life-threatening illnesses. Therefore, it is necessary to follow a set course of action to determine the nature of the masse and the most appropriate treatment. For example, testicular cancer which can present as a scrotal mass is a source of great concern and uniformly requires prompt intervention. Other masses, such as varicoceles, may be benign or cause testicular growth retardation in adolescent boys or impair fertility in adults. Thus, it is important for a patient to seek prompt medical attention when he identifies a scrotal mass or any lump or bump while performing a testicular self examination. The following information will assist you when talking to a urologist about varicoceles.
|
| |
|
What are varicoceles? |
|
|
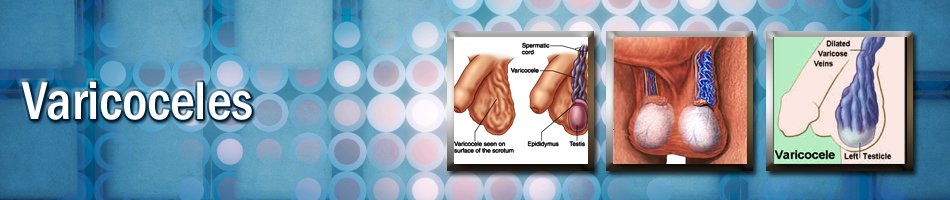
The spermatic cord is the structure that provides the blood supply to the testicle and contains the vas deferens which transports sperm from the testicle to the penis and urethra. The spermatic cord passes through the inguinal canal and continues into the scrotum. The pampiniform plexus is a group of interconnected veins, which drain the blood from the testicles and lies within the spermatic cord. The pampiniform plexus is believed to have an important functional role in maintaining testicular temperature in the appropriate range for sperm production. The pampiniform plexus cools blood in the testicular artery before it enters the testicles, helping to maintain an ideal testicular temperature, essential for optimal sperm production.
Varicoceles are abnormal enlargements (dilations) of the pampiniform plexus of veins within the scrotum. They are similar to varicose veins of the leg, and often form during puberty. They can become larger and thus more noticeable with time. Left-sided varicocoele are more common than right-sided varicocoele, likely due to anatomical differences between the two sides. Ten to fifteen percent of boys have a varicocoele. A fraction will develop testicular growth retardation during puberty.
|
| |
|
| What can cause varicoceles? |
|
|
Several causes of varicoceles have been suggested. Incompetent or absent valves within the spermatic veins may lead to pooling of blood from sluggish or even backflow. Additionally, the acute angle at which the left spermatic vein enters the renal (kidney) vein may transmit the relatively high pressure to result in backflow manifested in enlargement of the scrotal veins. This explains why varicoceles are more common on the left side since the gonadal vein on the left side enters the renal vein. The right gonadal vein is not as long and does not join with the right venal vein. Rarely, enlarged lymph nodes or other abnormal masses in the retroperitoneum (the space behind the abdominal cavity) will block the flow of blood in the spermatic veins, leading to acute enlargement of scrotal veins. This phenomenon is rare and is usually associated with pain.
|
| |
|
| How common are varicoceles? |
|
|
Varicoceles are present in an estimated 15 percent of all men. It is not know how many lead to infertility but approximately 40 percent of men undergoing evaluation for infertility are found to have a varicocoele and decrease sperm motility. There is no association other anomalies, race, geographic or ethnic origin.
|
| |
|
| What are the symptoms of varicoceles? |
|
|
Most men diagnosed with a varicocele have no symptoms, but varicoceles are important for several reasons. Varicoceles are thought to cause infertility and testicular atrophy (shrinkage). Approximately 40 percent of cases of primary male infertility and 80 percent of cases of secondary male infertility are believed to be due to varicoceles. Varicoceles rarely cause pain. When pain is present, it can vary from a dull, heavy discomfort to a sharp pain. The associated symptoms may increase with sitting, standing or physical exertion - particularly if any one of these activities occurs over long periods of time. Symptoms often progress over the course of the day, and they are typically relieved when the patient lies on his back, allowing improved drainage of the veins of the pampiniform plexus.
|
| |
|
| How are varicoceles diagnosed? |
|
|
Varicoceles can be discovered through self-examination or during routine physical examination. They may look or feel like a mass in the scrotum, and they have been described as having a "bag of worms" both because of their appearance and the way they feel. Physicians typically diagnose varicoceles with the patient in the standing position. The patient may be asked to take in a deep breath, hold it, and bear down while the physician feels the scrotum above the testicle. This technique, known as the Valsalva maneuver, assists the physician in detecting abnormal enlargement or increased fullness of the pampiniform plexus of veins. A physician may order a scrotal ultrasound test to help make the diagnosis, particularly if the physical examination is difficult or inconclusive. Radiographic hallmarks of varicoceles on scrotal ultrasonography are veins greater than three millimeters in size with reversal of blood flow within the veins of the pampiniform plexus during the Valsalva maneuver. In addition, the ultrasound study can provide testicular size measurements which are factored in the medical decision process in adolescents. However, routine radiographic screening for varicoceles in the absence of physical findings is not indicated.
|
| |
|
| What are the treatment options for varicoceles? |
|
|
Treatment of varicoceles is an appropriate consideration in patients with infertility, pain or testicular atrophy. No medical therapies are available for either treatment or prevention; however analgesic agents may alleviate associated pain when present.
There are two main approaches to the treatment of a varicocele:
Surgical Repair: This approach involves a variety of specific techniques, but all involve ligation (obstructing) of the spermatic veins thus interrupting blood flow in the vessels of the pampiniform plexus. The surgical approaches include open surgical repairs performed through a single 1 inch incision with or without the use of optical magnification (e.g., magnifying glasses or loupes or an operating microscope). Laparoscopic varicocele repair which utilizes telescopes passed through the abdominal wall are advocated by some. The open procedures are performed under a variety of anesthetics, from local to general anesthesia, whereas the laparoscopic approach is uniformly performed under a general anesthetic agent. With the advent of smaller incisions, which avoid muscle transection, the open procedures are becoming closer to the laparoscopic techniques in both speed of recovery and postoperative pain. Complications resulting from either open or laparoscopic approaches are rare, but include varicocele persistence/recurrence, hydrocele formation and injury to the testicular artery leading to loss of the testis (fortunately, this is an extreme complication).
Percutaneous Embolization: This procedure is performed by radiologists using a special tube that is inserted into a vein in either the groin or neck. After radiographic visualization of the enlarged veins of the pampiniform plexus, coils or balloons are released to create an obstruction (blockage) in the veins. This obstruction then typically leads to interruption of blood flow within the pampiniform plexus vessels and disappearance of the varicocele. Percutaneous embolization is typically performed with intravenous sedation anesthesia and usually takes several hours to complete. Complications may include varicocele persistence/recurrence, coil migration and complications at the venous access site. This has not been widely employed in most centers.
|
| |
|
| What can be expected after treatment? |
|
|
Recovery time after surgical repair is rapid. Pain is usually mild, and patients are asked to avoid strenuous activity for 10 to 14 days. Office work can typically be done one to two days after surgery. A follow-up visit with the urologist is scheduled. A follow-up semen analysis is obtained three to four months later if the procedure was performed to treat associated infertility. Open procedures performed with optical magnification have a low recurrence rate of approximately one percent.
Recovery time after embolization is also relatively short. Again, pain is typically mild, and patients are asked to avoid strenuous physical activity for seven to 10 days after the procedure. Patients may return to office work one to two days postoperatively. The recurrence rate with embolization is generally thought to be higher than that achievable with optical magnification. Nevertheless, there are circumstances when embolization may be preferable.
The impact of varicocele correction on fertility is not entirely clear. Some studies demonstrate improvement in fertility after varicocele repair, while other studies fail to document this change. Semen quality is improved in approximately 60 percent of infertile men undergoing correction of a varicocele, and this treatment should be considered in the context of other available treatment options as couples pursue therapy. In adolescents, where the main indication for surgery is testicular growth retardation, catch up growth occurs in over 90% of patients.
|
| |
|
| |
| Frequently asked questions: |
| |
| What will happen if I choose to observe my varicocele, rather than undergo treatment? |
|
|
Failure to treat a varicocele may result in testicular atrophy and/or a decline in semen quality. This may lead to infertility. The varicocele may, over time, lead to permanent, irreversible testicular injury.
|
| |
|
| I have pain with my varicocele. What can I do to help alleviate the pain? |
|
|
The use of adequate scrotal support (e.g., athletic supporter, briefs style underwear, etc.) can help the pain associated with a varicocele. Lying on your back facilitates varicocele drainage and often improves episodic discomfort as well. Use of analgesic agents (e.g., acetaminophen, ibuprofen, etc.) may be of benefit in treating the pain associated with a varicocele. Additionally, many patients obtain lasting relief of symptoms with varicocele correction through the above-mentioned techniques.
|
| |
|
| I am considering having my varicocele corrected for fertility reasons. How long will I have to wait to see improvement in semen parameters? |
|
|
Semen analyses are typically obtained at three to four month intervals after the procedure. Improvement is often seen within six months, but may not be observed until one year postoperatively.
|
| |
|
| My adolescent son was recently diagnosed with a varicocele. Should this be corrected? |
|
|
Indications for correction of a varicocele in an adolescent include disparity in testicular size exceeding 10% by volume. Additionally, correction is a consideration in patients with pain. Treatment of adolescents is highly individualized, and consultation with a urologist or a pediatric urologist to further discuss the appropriateness of treatment for a particular patient is highly recommended.
|
| |
|
| I am interested in fertility and have no symptoms. Should I have my varicocele repaired? |
|
|
Generally, asymptomatic varicoceles are not repaired. Most physicians do not believe there are health consequences of untreated asymptomatic varicoceles.
|
| |
|
| |
| |
|
| |
|
|
 |
Endoscopic removal of urinary stones: PCNL, URS, RIRS, CLT |
|
 |
LITHOTRIPSY (ESWL) |
|
 |
LASERS for stones and Prostate |
|
 |
Monopolar and bipolar TURP |
|
 |
HOLEP |
|
 |
Urodynamics and uroflowmetry |
|
 |
Laparoscopic urology surgeries |
|
 |
Paediatric urology surgeries |
|
 |
Urinary incontinence surgeries |
|
 |
Surgeries for genitourinary cancers |
|
 |
Reconstructive urology |
|
 |
Microsurgeries for infertility and impotence |
|
| |
|
| |
 |
|